Vaccinations in Pregnancy: Whooping Cough
Throughout our lives, the NHS offers safe and effective vaccines to protect us against infectious diseases.
That protection starts before birth, with the pertussis, or whooping cough vaccine, offered during pregnancy.
Cases of whooping cough have increased significantly in the UK this year. We want to encourage expectant mothers to get vaccinated against this potentially deadly illness.
What is Whooping Cough?
Whooping cough is a serious infection of the lungs and airways. It causes long bouts of uncontrolled coughing, which can make it hard to breathe and lead to choking and vomiting.
The “whoop” sound is caused by gasping for breath after each bout of coughing, though babies do not always make this noise.
It spreads very quickly, especially in newborns. Whooping cough can be severe and need hospital treatment. In some cases, it can be fatal.
Vaccinations in pregnancy give babies protection against whooping cough when they are most vulnerable.


The number of cases of whooping cough in the UK has increased significantly this year.
In May this year alone, there were 2,591 cases. That’s more than three times the total cases (858) inall of 2023.
Sadly, there have been eight infant deaths from whooping cough so far this year.


When to get Vaccinated against Whopping Cough
The best time to get vaccinated is between the 20th and 32nd week of pregnancy. This gives mother and baby the best protection.
The vaccine is usually offered through GP practices after the 20-week scan but can be given as early as 16 weeks.
It’s a 4-in-1 vaccine that protects against polio, diphtheria and tetanus.
By vaccinating women during pregnancy, immunity is passed to the unborn baby, protecting them until they are old enough to start their own course of NHS vaccinations.
This starts at eight weeks old, wth the NHS 6-in-1 vaccine, which protects against whooping cough, diphtheria, hepatitis B, Hib, polio, and tetanus.
Symptoms and Treatment
The first signs of whooping cough are like a cold, such as a runny nose and sore throat. After about a week, you or your child:
- will get coughing bouts that last for a few minutes and are worse at night
- may make a “whoop” sound – a gasp for breath between coughs (young babies and some adults may not “whoop”)
- may have difficulty breathing after a coughing bout and may turn blue or grey (young infants)
- may bring up a thick mucus, which can make you vomit
- may become very red in the face (more common in adults)
The cough may last for several weeks or months.
Babies under six months old with whooping cough have an increased chance of having problems such as:
- dehydration
- breathing difficulties
- pneumonia
- seizures (fits)
Whooping cough passes easily. You are most contagious from 6 days after your first symptoms to 3 weeks after you start coughing.
You should urgently see a Doctor or get help from NHS 111 if:
- Your baby is under six months old and has symptoms
- You or your child has a bad cough that is getting worse
- You’re pregnant and have been in contact with someone who has whooping cough.
Antibiotics are often given as treatment, but it will depend on age and how long you have had the cough.
Hospital treatment is usually needed if you have severe whooping cough or your baby is under six months old and has whooping cough.
Call 999 or go to A&E if:
- your or your child’s lips, tongue, face or skin suddenly turn blue or grey (on black or brown skin this may be easier to see on the palms of the hands or the soles of the feet)
- you or your child are finding it hard to breathe properly (shallow breathing)
- you or your child have chest pain that’s worse when breathing or coughing – this could be a sign of pneumonia
- your child is having seizures
The Full NHS Vaccine Schedule
The NHS vaccination programme protects against various diseases from childhood, adolescence, and old age.
Your child’s vaccines should be recorded in their ‘red book’. If you think your child may have missed a vaccination, feel free to contact your GP practice.
The NHS routine childhood immunisation programme was revised in September 2023. This is the new complete immunisation schedule.
| When | Diseases protected against | Vaccine given | Trade name | Usual site |
|---|---|---|---|---|
| 8 weeks old | Diphtheria, tetanus, pertussis (whooping cough), polio, Haemophilus influenza type b (Hib) and hepatitis B | DTaP/IPV/Hib/HepB | Infanrix hexa or Vaxelis | Thigh |
| Meningococcal group B (MenB) | MenB | Bexsero | Left thigh | |
| Rotavirus gastroenteritis | Rotavirus | Rotarix | By mouth | |
| 12 weeks old | Diphtheria, tetanus, pertussis, polio, Hib and hepatitis B | DTaP/IPV/Hib/HepB | Infanrix hexa or Vaxelis | Thigh |
| Pneumococcal (13 serotypes) | Pneumococcal conjugate vaccine (PCV) | Prevenar 13 | Thigh | |
| Rotavirus | Rotavirus | Rotarix | By mouth | |
| 16 weeks old | Diphtheria, tetanus, pertussis, polio, Hib and hepatitis B | DTaP/IPV/Hib/HepB | Infanrix hexa or Vaxelis | Thigh |
| MenB | MenB | Bexsero | Left thigh | |
| 1 year old (on or after the child’s first birthday) | Hib and Meningococcal group C (MenC) | Hib/MenC | Menitorix | Upper arm or thigh |
| Pneumococcal | PCV booster | Prevenar 13 | Upper arm or thigh | |
| Measles, mumps and rubella (German measles) | MMR | MMRvaxPro or Priorix | Upper arm or thigh | |
| MenB | MenB booster | Bexsero | Left thigh | |
| Eligible paediatric age group | Influenza (each year from September) | (each year from September) Live attenuated influenza vaccine LAIV | Fluenz Tetra | Both nostrils |
| 3 years 4 months old or soon after | Diphtheria, tetanus, pertussis and polio | dTaP/IPV | Boostrix-IPV | Upper arm |
| Measles, mumps and rubella | MMR (check first dose given) | MMRvaxPro or Priorix | Upper arm | |
| Boys and girls aged 12 to 13 years | Cancers and genital warts caused by specific human papillomavirus (HPV) types | HPV | Gardasil 9 | Upper arm |
| 14 years old (school Year 9) | Tetanus, diphtheria and polio | Td/IPV (check MMRstatus) | Revaxis | Upper arm |
| Meningococcal groups A, C, W and Y | MenACWY | Nimenrix | Upper arm | |
| 65 years old | Pneumococcal (23 serotypes | Pneumococcal polysaccharide vaccine (PPV23) | Pneumovax 23 | Upper arm |
| 65 years of age and older | Influenza (each year from September) | Inactivated influenza vaccine | Multiple | Upper arm |
| 65 from September 2023 | Shingles | Shingles vaccine | Shingrix | Upper arm |
| 70 to 79 years of age (plus eligible age groups and severely immunosuppressed) | Shingles | Shingles vaccine | Zostavax (or Shingrix if Zostavax contraindicated) | Upper arm |
Selective immunisation programmes
| Target group | Age and schedule | Disease | Vaccines required |
|---|---|---|---|
| Babies born to hepatitis B infected mothers | At birth, 4 weeks and 12 months old | Hepatitis B | Hepatitis B (Engerix B/HBvaxPRO) |
| Infants in areas of the country with tuberculosis (TB) incidence >= 40/100,000 | Around 28 days old | Tuberculosis | BCG |
| Infants with a parent or grandparent born in a high incidence country | Around 28 days old | Tuberculosis | BCG |
| Children in a clinical risk group | From 6 months to 17 years of age | Influenza | LAIV or inactivated flu vaccine if contraindicated to LAIV or under 2 years of age |
| Pregnant women | At any stage of pregnancy during flu season | Influenza | Inactivated flu vaccine |
| From 16 weeks gestation | Pertussis | dTaP/IPV(Boostrix-IPV) |
Additional vaccines for individuals with underlying medical conditions
| Medical condition | Diseases protected against | Vaccines required |
|---|---|---|
| Asplenia or splenic dysfunction (including due to sickle cell and coeliac disease) | Meningococcal groups A, B, C, W and Y | MenACWY MenB |
| Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) | |
| Influenza | Annual flu vaccine | |
| Cochlear implants | Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Chronic respiratory and heart conditions(such as severe asthma, chronic pulmonary disease, and heart failure) | Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Influenza | Annual flu vaccine | |
| Chronic neurological conditions (such as Parkinson’s or motor neurone disease, or learning disability) | Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Influenza | Annual flu vaccine | |
| Diabetes | Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Influenza | Annual flu vaccine | |
| Chronic kidney disease (CKD) (including haemodialysis) | haemodialysis) Pneumococcal (stage 4 and 5 CKD) | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Influenza (stage 3, 4 and 5 CKD) | Annual flu vaccine | |
| Hepatitis B (stage 4 and 5 CKD) | Hepatitis B | |
| Chronic liver conditions | Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Influenza | Annual flu vaccine | |
| Hepatitis A | Hepatitis A | |
| Hepatitis B | Hepatitis B | |
| Haemophilia | Hepatitis A | Hepatitis A |
| Hepatitis B | Hepatitis B | |
| Immunosuppression due to disease or treatment | Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) |
| Shingles vaccine | Shingrix – over 50 years of age | |
| Influenza | Annual flu vaccine | |
| Complement disorders (including those receiving complement inhibitor therapy) | Meningococcal groups A, B, C, W and Y | MenACWY MenB |
| Pneumococcal | PCV13 (up to 10 years of age) PPV23 (from 2 years of age) | |
| Influenza | Annual flu vaccine |
Extra vaccines may be offered to people with long-term health conditions or weakened immune systems.
As we said, the red book will have records of childhood vaccinations, as will the records held by GP surgeries. You may also see your jab history by logging into our online system.
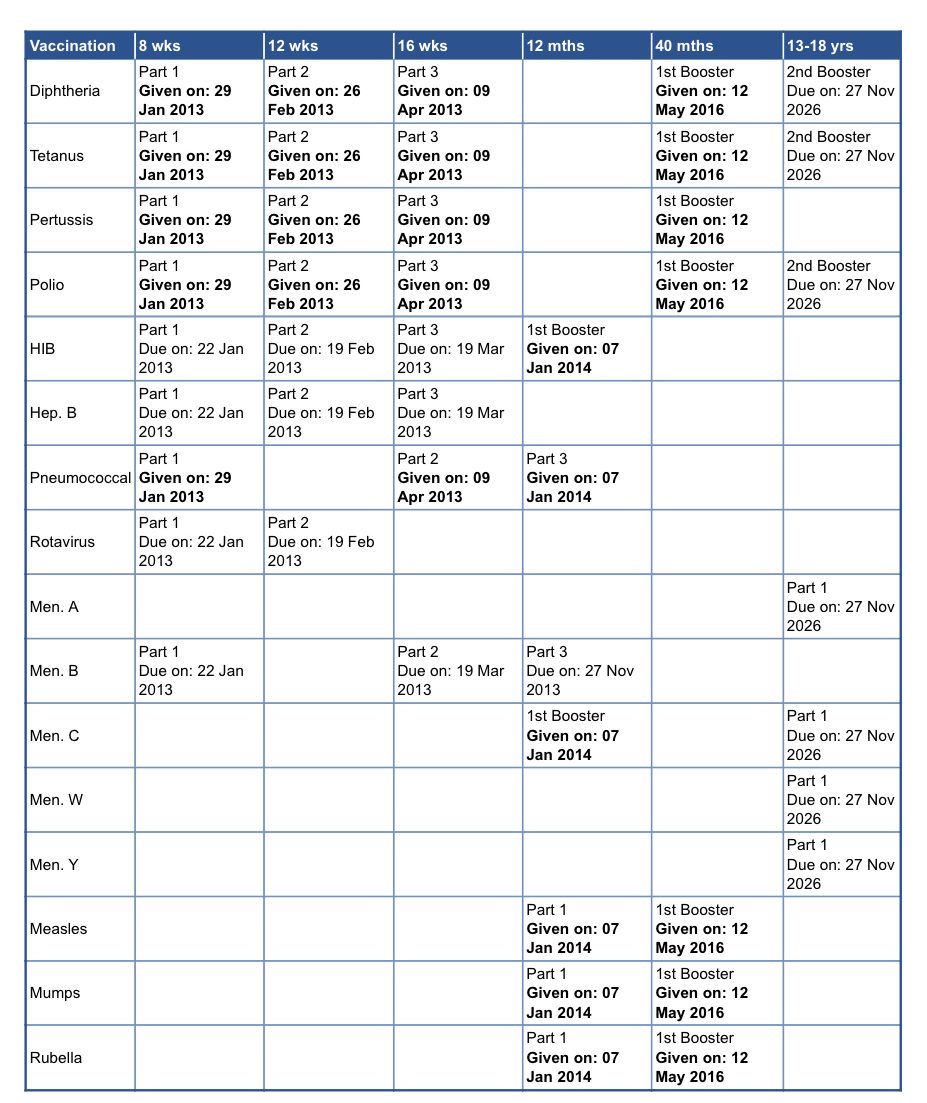
If you believe you, your child, or someone else you care for has missed any vital vaccinations, please get in touch with as soon as possible.
